
The ketogenic diet, primarily characterized by high fat and low carbohydrate intake, reduces epilepsy seizures by inducing ketosis and producing neuroprotective ketone bodies like beta-hydroxybutyrate (BHB). These ketones stabilize neuronal activity by enhancing GABA levels and reducing excitatory neurotransmitters. Additionally, the diet modulates gut microbiota, generates short-chain fatty acids like butyrate, and exhibits anti-inflammatory effects by decreasing markers such as TNF-α and IL-1β. Clinical studies demonstrate significant seizure reduction in 40-50% of pediatric patients, with some achieving near-total seizure control. For further detailed insights into the ketogenic diet's mechanisms and long-term efficacy, continue exploring.
Key Takeaways
- The ketogenic diet induces ketosis, producing ketone bodies that stabilize neuronal activity and reduce seizure frequency.
- Increased GABA levels and reduced excitatory neurotransmitters under the ketogenic diet help mitigate excessive neuronal firing.
- Ketone bodies enhance mitochondrial function and provide neuroprotective effects, raising seizure thresholds.
- The diet modulates gut microbiota, promoting short-chain fatty acids with neuroprotective and anti-inflammatory properties.
- Clinical evidence shows that 40-50% of children on the ketogenic diet experience significant seizure reduction.
Basics of the Keto Diet
The ketogenic diet, commonly referred to as the keto diet, is a meticulously structured nutritional regimen characterized by a macronutrient composition of high fat (70-80%), moderate protein (20%), and low carbohydrate (5-10%).
Central to the keto fundamentals is its distinctive macronutrient distribution, which necessitates rigorous adherence to dietary restrictions. The classical ketogenic diet mandates a precise ratio of 3-4 grams of fat for every 1 gram of carbohydrates and protein. This stringent balance is essential for inducing and maintaining a state of ketosis, where the body utilizes ketones, derived from fat, as the primary energy source instead of glucose.
Ketones serve as an alternative energy source for the brain, reducing neuronal excitability and enhancing GABA production. Initially developed in the 1920s for the therapeutic management of epilepsy, particularly in pediatric populations with drug-resistant epilepsy, the diet has demonstrated substantial efficacy in seizure reduction.
This necessitates thorough meal planning and continuous monitoring to maintain the delicate macronutrient equilibrium. The classical form of the diet is often accompanied by variants such as the Modified Atkins Diet (MAD), which offer more flexibility while still adhering to the core principles of keto fundamentals.
These dietary restrictions are critical for achieving and sustaining the diet's therapeutic benefits, particularly in the context of epilepsy management.
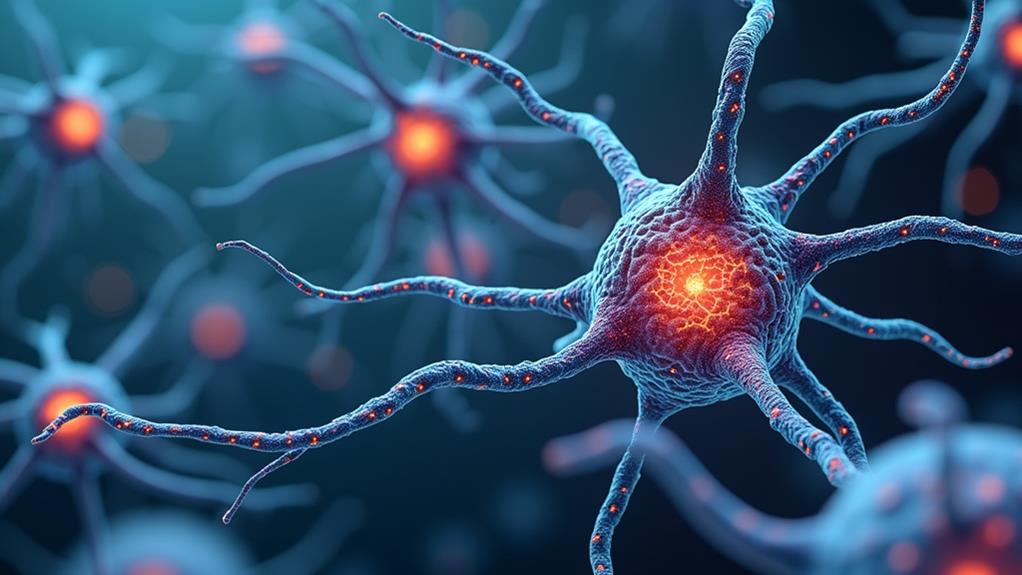
Mechanism of Ketosis
The ketogenic diet induces ketosis by shifting the body's primary energy source from glucose to fat, resulting in the production of ketone bodies such as beta-hydroxybutyrate.
These ketone bodies serve as an alternative brain energy source, exhibiting neuroprotective properties that stabilize neuronal activity and raise the seizure threshold.
Additionally, the metabolic state of ketosis enhances gamma-aminobutyric acid (GABA) levels while reducing excitatory neurotransmitters, thereby mitigating excessive neuronal firing linked to seizures.
Ketone Body Production
How does the ketogenic diet facilitate ketone body production? The ketogenic diet, characterized by a high-fat, low-carbohydrate composition, induces a metabolic state known as ketosis.
In ketosis, the body shifts its primary energy source from glucose to fats, leading to increased ketone metabolism. This metabolic adaptation results in the production of ketone bodies, including beta-hydroxybutyrate (BHB), acetone, and acetoacetate, in the liver through fatty acid oxidation.
The elevation of BHB, a principal ketone body, is particularly significant due to its neuroprotective properties. Research indicates that BHB can increase the seizure threshold, potentially stabilizing neuronal activity.
Additionally, this shift in energy metabolism is associated with reduced excitatory neurotransmitter activity and enhanced levels of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter. The resultant balance between excitatory and inhibitory neurotransmitters contributes to the reduction in seizure frequency observed in individuals on a ketogenic diet.
Clinical evidence supports the efficacy of this dietary intervention, with approximately 40-50% of pediatric patients experiencing a significant decrease in seizure frequency.
The ketone benefits therefore underscore the therapeutic potential of the ketogenic diet in managing epilepsy.
Brain Energy Source
During ketosis, the brain undergoes a significant metabolic shift, utilizing ketone bodies as its primary energy source instead of glucose. This energy conversion is critical in altering brain metabolism, especially for patients with epilepsy. Ketone bodies, such as beta-hydroxybutyrate, are produced through the metabolism of fats and offer multiple neuroprotective benefits. These benefits include stabilization of neuronal excitability and enhancement of mitochondrial function, both of which can contribute to the reduction of seizure activity.
Key mechanisms through which ketosis aids in seizure control include:
- Increased GABA Production: Elevated levels of GABA, an inhibitory neurotransmitter, help to calm neuronal firing and increase the seizure threshold.
- Reduction of Excitatory Neurotransmitters: The ketogenic diet decreases the production of excitatory neurotransmitters like aspartate, stabilizing synaptic activity in the brain.
- Neuroprotective Effects of Ketone Bodies: Ketone bodies stabilize neuronal excitability and enhance mitochondrial function, reducing seizure frequency.
Clinical evidence indicates that children adhering to the ketogenic diet experience a significant reduction in seizures, with over 50% achieving at least a 50% decrease in seizure frequency.
This robust evidence underscores the efficacy of the ketogenic diet in modifying brain metabolism and improving seizure control.
Impact on Neurotransmitters
Adopting a ketogenic diet (KD) has shown profound effects on neurotransmitter dynamics, essential for managing epilepsy. The KD markedly modulates neurotransmitter balance by increasing gamma-aminobutyric acid (GABA) levels, an inhibitory neurotransmitter pivotal for stabilizing neuronal excitability and reducing seizure activity. Enhanced GABAergic transmission leads to a higher seizure threshold, contributing to seizure control.
Furthermore, the KD decreases the levels of excitatory neurotransmitters such as aspartate, thereby reducing hyperexcitability in the brain. This dual modulation—elevating inhibitory neurotransmitters while diminishing excitatory ones—promotes a favorable balance between excitation and inhibition within the central nervous system, critical for mitigating epileptic seizures.
Additionally, the ketone bodies produced during ketosis enhance mitochondrial function, supporting neuronal health and optimizing energy metabolism in the brain. Improved mitochondrial efficiency further sustains the neurotransmitter balance, reinforcing neuronal stability and resilience against epileptic activity.
Clinical evidence supports the efficacy of the KD in seizure management, with studies indicating that 40-50% of pediatric patients experience at least a 50% reduction in seizure frequency. These findings underscore the KD's role in markedly improving seizure control through its impact on neurotransmitter dynamics.
Modulation of Gut Microbiota
The ketogenic diet's modulation of gut microbiota is pivotal in influencing the gut-brain axis, with alterations in microbiome composition facilitating enhanced ketone production and metabolic stability.
This shift promotes the generation of short-chain fatty acids, such as butyrate, which have been shown to exert neuroprotective effects and mitigate seizure frequency.
Additionally, the reduced pro-inflammatory cytokine environment supports neuronal excitability stabilization, underscoring the diet's potential in managing epilepsy.
Gut-Brain Axis Impact
Modulation of the gut microbiota by the ketogenic diet (KD) may present a significant mechanism in its efficacy for seizure management in epilepsy. Research underscores that the KD influences gut health by enhancing microbial diversity, which is essential to neurological stability.
The shift in gut microbiota composition under KD fosters beneficial bacteria, leading to metabolic changes that may strengthen seizure protection. The gut-brain axis is important in this situation, with KD-induced changes promoting the production of short-chain fatty acids (SCFAs).
These SCFAs exhibit anti-inflammatory properties, potentially reducing pro-inflammatory cytokines in the gut. The consequent stabilization of synaptic excitability could raise the seizure threshold, offering a clinical advantage in epilepsy management.
Key Mechanisms Involved:
- Enhanced Microbial Diversity: KD increases the variety of beneficial gut bacteria, positively impacting gut health and brain function.
- Anti-inflammatory Effects: The production of SCFAs reduces gut inflammation, which may contribute to lower seizure frequencies.
- Synaptic Stabilization: Reduction in pro-inflammatory cytokines can stabilize neuronal activity, thereby raising seizure thresholds.
Therefore, the interplay between gut microbial modulation and the gut-brain axis underscores a significant pathway through which the KD may exert its anticonvulsant effects.
Microbiome Ketone Production
Several lines of evidence suggest that the ketogenic diet (KD) markedly modulates gut microbiota, leading to increased production of ketone bodies that may play an important role in seizure control. The KD alters the composition of the gut microbiota, fostering beneficial bacteria that enhance metabolic processes associated with seizure reduction. Specifically, the diet promotes the growth of bacterial species like Akkermansia muciniphila, linked to improved gut barrier function and reduced systemic inflammation, both significant in managing seizure activity.
The bacterial fermentation of dietary fibers results in the production of short-chain fatty acids (SCFAs), compounds known for their neuroprotective and anti-inflammatory effects. These SCFAs contribute to the modulation of microbiome diversity and may play a role in reducing seizure frequency.
In addition, the increased ketone body levels resulting from these microbiota changes serve as an alternative energy source for neurons, potentially stabilizing neuronal excitability and reducing seizure propensity.
Additionally, the modulation of the gut microbiota through the KD can influence the production of neurotransmitters such as gamma-aminobutyric acid (GABA), vital for inhibiting seizure activity. Collectively, these microbiota-mediated mechanisms underscore the therapeutic potential of the KD in epilepsy management.
Anti-Inflammatory Effects
Curiously, how does the ketogenic diet (KD) confer its anti-inflammatory benefits in the context of epilepsy management? The KD effectively modulates neuroinflammation markers and cytokine activity, leading to reduced seizure frequency.
Key mechanisms include:
- Cytokine Modulation: The KD increases levels of anti-inflammatory cytokines while decreasing pro-inflammatory markers such as TNF-α and IL-1β. This modulation stabilizes neuronal activity, reducing seizure susceptibility. It has also been shown to improve blood sugar control, which is linked to lower inflammation levels.
- NLRP3 Inflammasome Inhibition: Ketone bodies produced during ketosis inhibit the activation of the NLRP3 inflammasome, a critical component in neuroinflammation. This inhibition reduces neuroinflammatory responses, thereby providing neuroprotection.
- Oxidative Stress Reduction: The KD decreases oxidative stress markers, which are closely linked to inflammation and neuronal damage. Reduced oxidative stress contributes to the stabilization of neuronal cells, mitigating seizure activity.
Additionally, the KD's influence on gut microbiota plays a pivotal role. A balanced gut flora produces short-chain fatty acids that foster an anti-inflammatory environment in the central nervous system.
This multifaceted approach underscores the KD's potential as a therapeutic strategy in epilepsy management by targeting and reducing neuroinflammation.
Clinical Evidence and Studies
The ketogenic diet (KD) has garnered significant clinical interest due to its robust efficacy in reducing seizure frequency among patients with drug-resistant epilepsy. Clinical studies have demonstrated that approximately 40-50% of children adhering to the KD experience at least a 50% reduction in seizure frequency, with about 10-20% achieving over 90% reduction.
Importantly, a thorough review of research spanning from 2009 to 2022 has substantiated the diet's significant impact on seizure reduction, especially in conditions such as Dravet syndrome and infantile spasms.
The classical KD, characterized by a 4:1 fat to protein plus carbohydrate ratio, has shown equivalent effectiveness in managing seizure activity as newer dietary approaches like the Modified Atkins Diet (MAD). This assertion is supported by a meta-analysis revealing that children on the KD exhibit substantial improvements in seizure control.
Additionally, various studies indicate that up to 15% of children can attain complete seizure freedom through this dietary regimen.
In addition to seizure reduction, some evidence suggests that the KD may enhance cognitive outcomes in pediatric patients.
Collectively, these clinical findings underscore the KD's potential as a potent therapeutic strategy for drug-resistant epilepsy.
Risks and Side Effects

Adherence to the ketogenic diet (KD) is not without its potential risks and side effects, necessitating a careful and monitored approach. Due to its high-fat content, the KD can lead to several long-term health issues. Common risks include:
1. Low Bone Density: Prolonged use of the KD can result in decreased bone mineral content, making bones more susceptible to fractures.
2. Constipation and Gastrointestinal Issues: Initial phases of the diet often bring about symptoms such as diarrhea, vomiting, and loss of appetite, which may require specific dietary adjustments.
Additionally, staying hydrated and maintaining electrolyte balance with potassium and magnesium-rich foods can help mitigate these issues.
3. Increased Cholesterol Levels: The high-fat nature of the diet can contribute to heightened lipid profiles, necessitating regular blood tests for nutritional monitoring.
Children on the KD may face additional challenges, such as slower growth rates and an increased risk of kidney stones. Consequently, continuous monitoring by healthcare providers is essential. Regular blood and urine tests are fundamental to detect and manage nutritional deficiencies and side effects.
Moreover, individuals may experience sluggishness and fatigue as their bodies shift to using ketones for energy instead of carbohydrates. These symptoms typically improve over time but underscore the importance of close nutritional monitoring.
Effective management and dietary adjustments are significant to maintaining the diet's safety and efficacy.
Long-Term Outlook and Management
Long-term management of epilepsy through the ketogenic diet (KD) necessitates a thorough, evidence-based approach to guarantee sustained efficacy and mitigate potential adverse effects. Approximately 40-50% of children on the KD experience a 50% reduction in seizures, with 10-20% achieving over 90% reduction, demonstrating its significant long-term effectiveness.
This underscores the importance of dietary adherence strategies, which include regular consultations with healthcare providers to monitor nutritional status and identify risks such as low bone density, kidney stones, and high cholesterol. The Mediterranean diet is often preferred for its flexibility and variety, suggesting that balanced, varied diets are important for sustainable diabetes management.
Regular medical follow-ups are imperative to address these potential complications. If seizure control is sustained for two or more years, healthcare providers might recommend a gradual tapering off the KD, though some families opt to continue for enhanced seizure management.
Adjusting off the diet requires medical supervision to avert seizure exacerbation, and maintaining anti-seizure medications during this period is often necessary.
Caregiver support plays an essential role in ensuring successful long-term management, necessitating collaboration with dietitians and epilepsy organizations. This integrated approach aids in maneuvering the complexities of the KD, ensuring both efficacy in seizure reduction and the minimization of adverse effects over time.
Frequently Asked Questions
How Does the Keto Diet Work for Epilepsy?
The keto diet works for epilepsy by inducing ketosis, which stabilizes neuronal activity through increased GABA levels, improved mitochondrial function, and reduced inflammation. These keto mechanisms are effective across various seizure types, particularly in drug-resistant cases.
How Long Does It Take for Keto to Stop Seizures?
The keto duration to impact seizure frequency typically ranges from 2 to 4 weeks, with some patients requiring up to three months. Approximately 40-50% experience significant seizure reduction within this period, depending on individual factors and adherence.
Why Do Ketone Bodies Reduce Seizures?
Ketone metabolism provides an alternative brain energy source, stabilizing neuronal function. This process enhances gamma-aminobutyric acid (GABA) levels, reduces aspartate, and modulates neurotransmitter dynamics, contributing to decreased neuronal excitability and seizure thresholds.
What Foods Help With Epilepsy Seizures?
Dietary considerations for epilepsy seizures include meal planning with high-fat foods like butter and olive oil, low-carbohydrate vegetables such as spinach, and moderate protein sources like eggs, while avoiding high-carbohydrate foods to maintain therapeutic ketosis.
Conclusion
The ketogenic diet exerts multifaceted effects that contribute to the reduction of epilepsy seizures. These effects include the induction of ketosis, modulation of neurotransmitter activity, alteration of gut microbiota, and anti-inflammatory properties. Clinical evidence supports its efficacy in seizure control, yet potential risks and side effects necessitate careful management. Long-term adherence to the diet may offer sustained benefits, but requires continuous monitoring to mitigate adverse outcomes and guarantee nutritional adequacy.








No Comments